“Xylazine is making the deadliest drug threat our country has ever faced, fentanyl, even deadlier,” said DEA administrator Anne Milgram in a public safety alert. “DEA has seized xylazine and fentanyl mixtures in 48 of 50 states. The DEA Laboratory System is reporting that in 2022 approximately 23% of fentanyl powder and 7% of fentanyl pills seized by the DEA contained xylazine.”
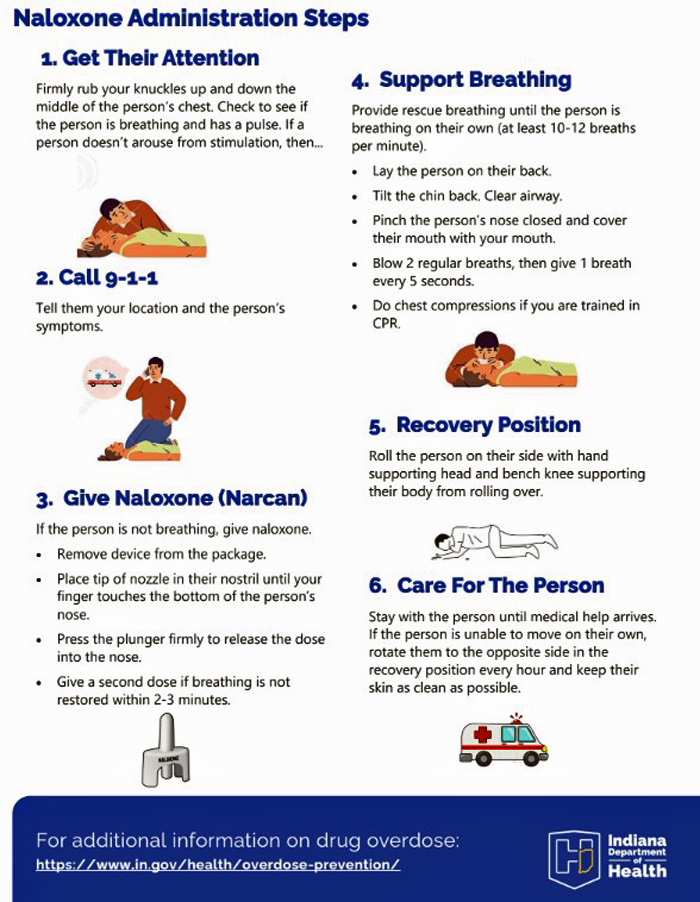
The Pulaski County Health Department warns that Narcan cannot reverse the effects of xylazine. However, because xylazine is almost always found in combination with opioids, including fentanyl, naloxone should still be administered whenever an opioid overdose is suspected.
The Indiana Department of Health has issued new information this week about xylazine, and the local health department has shared it as follows:
Xylazine (“Tranq”) is in Indiana
What is tranq and why are people using it?
Tranq or tranq dope are terms used to refer to xylazine, which is a commonly used veterinary sedative. It is not intended for human use but has shown up in the illicit drug market throughout Indiana and nationwide. It is often mixed and sold with fentanyl, as well as other opioids, and it also has been seen in cocaine and meth. People have described the effects like being knocked un-conscious for several hours, sometimes days. Some people use it because its effects last longer than fentanyl, allowing them to use less often or last over-night. Some people are using it unintentionally because they don’t know it’s in the drug supply.
What do you need to know
- Xylazine can knock people out for an extended period of time. During that time, people have no recollection of what happened and sometimes pass out in dangerous places, such as roadside curbs, as well as in dangerous positions, blocking breathing and blood circulation. Making a safety plan, using a buddy system, and using in a safe place could prevent injuries.
- Xylazine does not respond to naloxone because it is not an opioid. Naloxone should still be ad-ministered since the person may have taken drugs that contain opioids. When a person has used xylazine in combination with an opioid it can be hard to see when the naloxone has become effective. The person may start breathing again after naloxone has been administered but the person may still remain unconscious when xylazine is in their system. Be sure to check for breathing after administering naloxone. If someone isn’t breathing, give rescue breaths.
- Wounds can become very serious and painful. If you think you have used xylazine and start to see dark coloration, smell foul odor, and/or experience extreme pain, you should seek medical assistance. If you feel comfortable, communicate that you may have been exposed to xylazine, it is critical for medical professionals to know so they can treat the wound properly.
- Xylazine withdrawal is different from opioid withdrawal. If xylazine is something you use frequently or if you use opioids containing xylazine frequently, you may have withdrawal symptoms from both xylazine and opioids. While buprenorphine/methadone can control your opioid withdrawal symptoms, these medications won’t control withdrawal from xylazine. Xylazine withdrawal can cause significant anxiety, currently there are not good medications to manage this type of withdrawal. Be very careful when using any other substances such as clonidine or benzos to counteract the anxiety, as it increases your risk of overdose.
How do I know if I used xylazine?
People report losing track of large amounts of time and not remembering what happened to them. Community members say seeing someone on “tranq” is like seeing someone walk around like a zombie. People who regularly use opioids report being unable to work or stay awake when using xylazine, even passing out before they are in a safe space.
Who should I talk to?
If you believe you have used xylazine and want to learn more or get support, you could go talk to your local harm reduction program (if available). You may also seek peer recovery support or other resources for social and medical support. Some harm reduction programs have on-site clinical staff that can help, but emergency medical attention could save your life depending on the severity of your wounds.
Anything else?
We are still learning how xylazine affects people and sharing your experience could help save lives. Most of the information we have gathered has come from firsthand experience. Learn more about harm reduction programs in Indiana.
Wound Care
Xylazine has been associated with wounds that spread and worsen quickly. The wounds have been seen to occur regardless of how people use xylazine: smoking, snorting, injecting, and wounds are showing up in places outside of the area of injection. People report xylazine wounds from drug injection initially start as small superficial red blister(s). If not kept clean, moistened, and covered then they can worsen and spread. Wounds can look like burns with black, dead tissue and often have a foul order associated with them. It is important to keep them covered and keep tissues soft while they heal.
When caring for xylazine associated wounds:
- Wash with water: Wash with warm water and soap if possible (or just water).
- Keep wounds covered: Use Xeroform bandages or a thin layer of Vaseline on gauze work best for coverage.
- Avoid touching your hands or injecting in that area.
- Repeat until healed: Every 1-2 days repeat the washing and covering process.
Seek immediate medical attention for your wounds if: they turn black, have a foul odor, bones or muscles become visible, chunks of tissue fall off, and/or you experience fever or chills.
 |